Medicine
A cockpit for tissue medicine
Probably no medical field has felt the change of time as strongly as pathology: Soon, the diagnostic experts will leave their microscopes – and instead settle in the futuristic-looking Pathojet invented at the University of Bern.

Pathology is – literally translated from ancient Greek – the teaching of illnesses. In the past, experts often held inquests in order to deepen their knowledge of the disease processes. “Unfortunately, our field is still associated with autopsies today,” says Alessandro Lugli, Chief Physician for Gastrointestinal Tissue Medicine. “However, due to the higher level of medical knowledge and the new technologies that are available to us, this activity is increasingly taking a back seat.” And Heather Dawson, Chief Physician of Tissue Medicine , adds: “I haven’t performed a single autopsy in ten years.”
New institute name
Lugli and Dawson both work at the Institute of Tissue Medicine and Pathology at the University of Bern, which changed its name at the beginning of the year in order to underline the far-reaching change that is visibly transforming the field of pathology. Unlike their colleagues who treat sick people, tissue medicine specialists are not in direct contact with patients. They use tissue samples to make an in-depth diagnosis, so to speak, behind the scenes.
“I haven’t performed a single autopsy in ten years.”
Heather Dawson
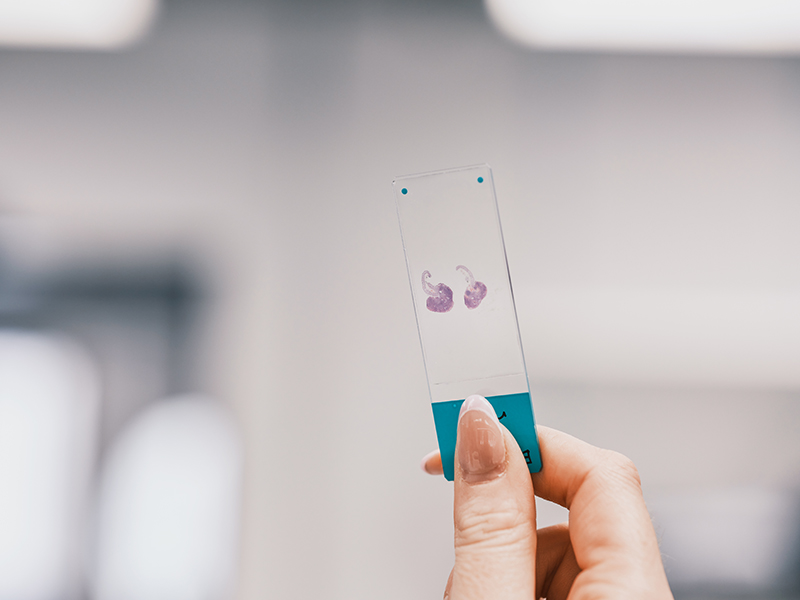
Wafer-thin slices
Now Dawson uses her badge to open the door to a bright room, which is incredibly spacious and in which there is both a concentrated calm and a busy hustle and bustle. A good dozen people are busy using chemical methods to extract water from the approximately 700 different tissue samples that are processed here every day, then encapsulate them in paraffin blocks – and then cut them into wafer-thin slices that are about 30 times thinner than a human hair.
“In paraffin, a type of candle wax, not only the structures but also the biological molecules, such as DNA and proteins, are preserved for decades,” Dawson explains. From the cutting block, the tissue slices are carefully placed in a water bath, where they float on top – and reach a glass slide when pulled out of the water at the right angle.
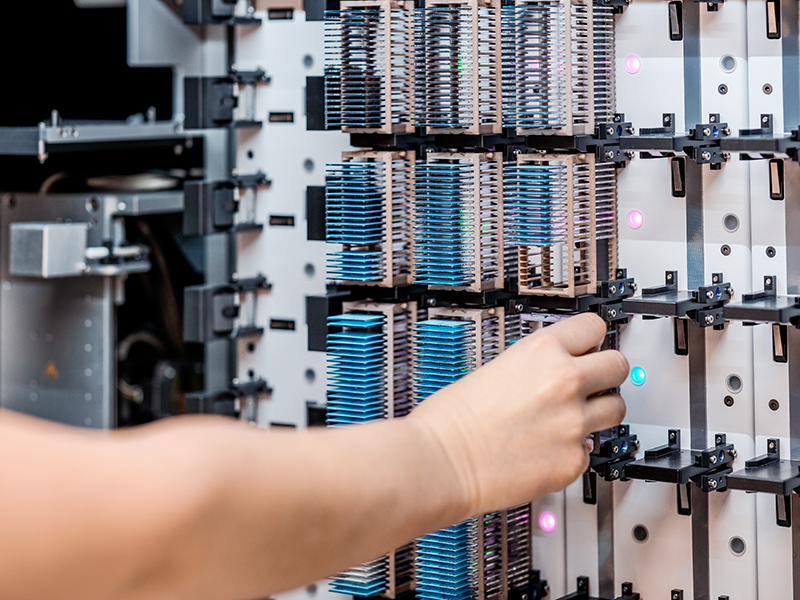
“Then the tissue sections enter the staining area,” says Dawson, pointing to the machine park, where the glass slides are transferred from one bath to the next by small robot arms at precisely defined intervals. “We optimized the processes and also carefully considered where we would place the machines so that the samples only move in one direction,” Dawson explains. “Today, a sample still travels a 50-meter journey while it is being processed. Before optimization, the journey was ten times longer due to the back and forth.”


Microscopy rooms in the diagnostic wing
Finally, the stained sections are sent to the distribution station, where they are assigned to the various doctors who cover different areas of tissue medicine with their expertise. And who, in six different microscopy rooms in the adjoining diagnostic wing, see whether a tissue sample contains cancer cells, for example (and if so, whether the cancer has already colonized lymphatic vessels and thus started to spread to other parts of the body).
At the distribution station there is an inconspicuous box about two meters high with a transparent glass wall. “This is the scanner: the interface to digitalization – and artificial intelligence,” says Lugli. Currently, only a portion of the tissue sections are scanned because the machine’s capacity is limited. But due to the rapid advances in technology, Lugli predicts that this will change in just a few years’ time.
Loss of status symbol
At the latest, that is when microscopes will no longer be needed. “As a result, we lose our status symbol in pathology,” says Lugli with a mischievous smile. He invented the Pathojet to help his colleagues overcome this loss – and at the same time to prepare them for the future in the best possible way. “I’m a huge movie fan and was inspired by “Top Gun”,” says Lugli.
“I’m a huge movie fan and was inspired by “Top Gun.”
Alessandro Lugli
Just as Tom Cruise thunders through the air in daring maneuvers, Lugli’s colleagues are also to be able to glide over the stained cell clusters in low flight thanks to a type of medical cockpit – and detect diseased tissue. The new digital working area has to be ergonomic so that specialists can maintain their concentration for hours if need be.
“I actually had the idea back in 2014, but it didn’t come off the shelf for several years because none of the industry partners I approached in order to implement it believed in the idea,” says Lugli. Then, things got rolling when Miryam Blassnigg joined the Institute of Tissue Medicine and Pathology as assistant to the director. She had previously held various positions in the private sector – and immediately took up the challenge. “I like to initiate and implement things,” says Blassnigg.
Because tissue physicians spend a large part of their work and many hours examining images of tissue sections for suspicious abnormalities, Blassnigg looked in other sectors for chairs people use for hours – with as few complaints as possible. “That’s how I came up with gaming chairs,” says Blassnigg.
Upholstered reclining chair instead of a tense neck
In terms of appearance and functionality, she particularly liked a product from Canada whose manufacturer also sells flight simulators and workstations for remote control of self-propelled mine vehicles. Once Blassnigg and Lugli had contacted the manufacturer, things all of a sudden went quickly. “They were very motivated and worked hard to develop a prototype together with us,” says Blassnigg.
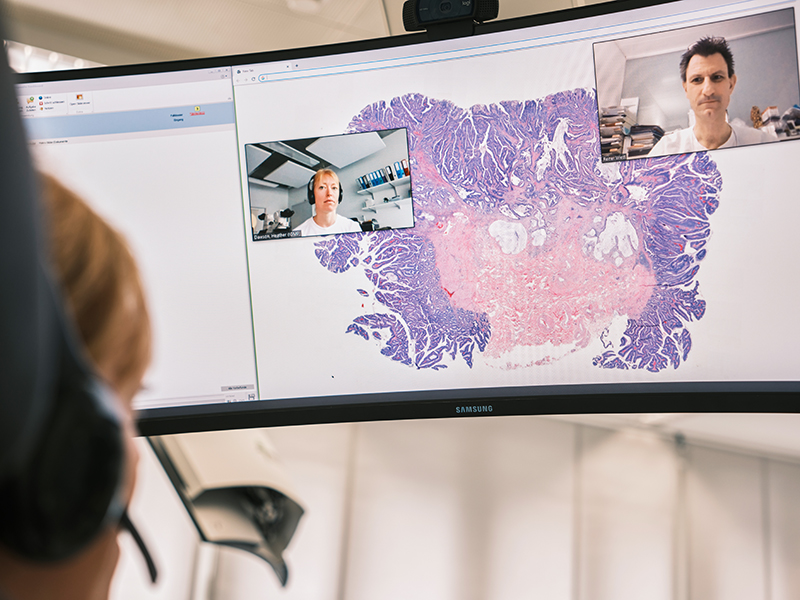
Today, three of these futuristic-looking workstations are located in the test diagnostics room of the Institute. “I feel like I’m in a bubble in the Pathojet and can focus very well on the images,” says Lugli. “Digitalization also gives me more options and I can also use artificial intelligence for image analysis, for example.” Dawson, too, has much to gain from the workplace of the future: Instead of staring into the eyepiece of a microscope with a curved back and visibly tense shoulder and neck areas, the tissue physician can flop into an ergonomically upholstered reclining chair.
“I can also use artificial intelligence for image analysis, for example.”
Alessandro Lugli
The rounded steel frame of the Pathojet sticks forward like a scorpion’s tail high above the chair – and presents the pilots in the cockpit with all the information they need to visually assess the digitalized tissue sections on a wide curved screen. “In the Pathojet, different colored sections can be placed next to each other and compared,” says Dawson. “And we can discuss our conclusions right away with the colleagues who are waiting for our results to proceed with treatment.”
World’s first device of its kind
Now Reiner Wiest is connected via video call. The Head of Gastroenterology at Inselspital would like to discuss with Dawson the findings of the patient from whom he had previously removed the polyp during the colonoscopy. On the stained sections of the intestinal polyp, Dawson quickly recognizes that it is an early-stage colon cancer with no risk factors. “The patient is cured with the complete removal of the polyp,” says Dawson.
With the choice of the new name, which puts tissue medicine in the spotlight, the institute has taken on a pioneering role. Likewise, the Pathojet, registered as a trademark of the University of Bern, is the world’s first device of its kind in this field. Last autumn, Lugli and Blassnigg presented the Pathojet to the public for the first time at the European Congress of Pathology in Basel. “It was a huge success. The Pathojet impressed not only with its ergonomics and design, but also with its cost-effectiveness,” says Blassnigg. And Lugli adds: “People stood in line, everyone wanted to sit in it.”
About the person

Heather Dawson
is a senior physician at the Institute of Tissue Medicine and Pathology. After training as a specialist in Bern and Lucerne and a research stay in Canada, she returned to head up the dermatopathology group and the Laboratory for Histological Diagnostics. She is also responsible for bone and soft tissue tumors and conducts research into prognostic biomarkers in colorectal carcinoma. Since 2017, she has headed up the Swiss Section of the International Academy of Pathology.
Contacts:
PD Dr. med. Heather Dawson, Senior Staff Pathologist, heather.dawson@unibe.ch
Prof Dr. med. Alessandro Lugli, Chief Physician, alessandro.lugli@unibe.ch
Miryam Blassnigg, Assistant to the Director, miryam.blassnigg@unibe.ch
The online magazine of the University of Bern

Subscribe to the uniAKTUELL newsletter
The University of Bern conducts cutting-edge research on topics that concern us as a society and shape our future. In uniAKTUELL we show selected examples and introduce you to the people behind them – gripping, multimedia and free of charge.
New magazine uniFOKUS
Subscribe free of charge now!
This article first appeared in uniFOKUS, the new University of Bern print magazine. Four times a year, uniFOKUS shows what academia and science are capable of. Thematically, each issue focuses on one specialist area from different points of view and thus aims to bring together as much expertise and as many research results from scientists and other academics at the University of Bern as possible.
