Medical technology
Practising delicate brain procedures
At the world's first 4D neurosurgery simulation workshop, specialists from all over Europe honed their surgical techniques in Bern. With realistic models of dilated cerebral arteries, a new training standard is to be established to increase patient safety.

The deep red expansion of the blood vessel winding through the vulnerable brain tissue is clearly visible on the screen. The surgical instruments are lined up on the table next to the new simulator. There are fine tweezers and instruments used to push away and spread the brain convolutions, but also special clamp holders.
The world's first simulation workshop
Now Diamantoula Pagkou clamps a slightly curved clip into the holder. She has travelled from Greece to Bern to participate – together with 18 other neurosurgeons from Germany, Italy and Switzerland – in the world's first simulation workshop for operations on blood vessels in the brain.
She guides the opened clip with a steady hand to the balloon-like widening of the cerebral artery, the so-called aneurysm. It is important to place the clip in such a way that it separates the aneurysm from the artery – and at the same time does not obstruct the blood flow into the three branches that leave the artery at the dilated site.
Weak points in the blood vessel walls
Aneurysms are weak points in the blood vessel walls that give way to pressure and bulge outwards. They are estimated to occur in two to three percent of the population – that's about 24 million people in the EU. Aneurysms probably develop more often than average in people who smoke, suffer from high blood pressure or kidney cysts, have certain genetic characteristics, and in middle-aged women.
Usually, aneurysms do not cause any symptoms, and are often discovered as accidental findings. But when they rupture or burst, they cause a severe cerebral haemorrhage that requires emergency treatment. About 30 percent of all patients die from the haemorrhage or its consequences, and only just under 20 percent survive the haemorrhage without damage.

Whether an aneurysm bursts or not depends on many factors. The risk is particularly high with very extensive aneurysms and those that form daughter bubbles. In such cases, surgery is recommended to close the aneurysm – and prevent it from bursting.
Unique shape and form
However, these operations are among the most delicate procedures in Neurosurgery: "If you accidentally clamp something wrong, part of the brain dies within a few minutes," says Andreas Raabe, chief physician and director of the Department of Neurosurgery at Inselspital. To make matters worse, every aneurysm is unique in its shape and form – and therefore has to be operated on differently.
For some years now, thanks to impressive technical advances, it has been possible to repair small aneurysms with a catheter that is inserted into the thigh. "But at the same time, technical progress also means that prospective neurosurgeons today gain less surgical experience during their training than they did twenty years ago", says Raabe.
Elevated blood pressure in the surgical model
In the seminar room of the workshop, Pagkou has just set the clip – and asks Raabe for an assessment. He takes the fine surgical instruments in hand, sits down at the microscope – and gently moves the clipped aneurysm back and forth to inspect it from all sides. "The clip is well placed, but look," says Raabe, pointing to the screen: "This leaves a small part of the dilated area unclipped. This part could grow again, we want to avoid that."

Then he removes the clip – and attaches two other clips to the small balloon at different angles. Now David Bervini, who had earlier given feedback on the simulated operation to another workshop participant at the neighbouring unit, joins the group. Bervini is a senior physician in neurosurgery at the Inselspital; he conceived and organised the workshop together with Raabe.
Bervini taps on the screen of the simulation robot – and increases the blood pressure in the surgical model. The clips begin to move at a pulse rate. But the aneurysm remains still. "Completely severed, this is good," says Bervini. Raabe explains that when operating on complex aneurysms, one should think less about individual clips and more about a combination of clips.
Realistic mapping in space and time
And Bervini explains that when planning the operation, you also have to take into account how you bed the patient – and in which direction you turn the head. Because during an operation you have to access an aneurysm from above: this way, gravity, which pulls the flabby brain mass downwards, helps to expose the affected blood vessel.
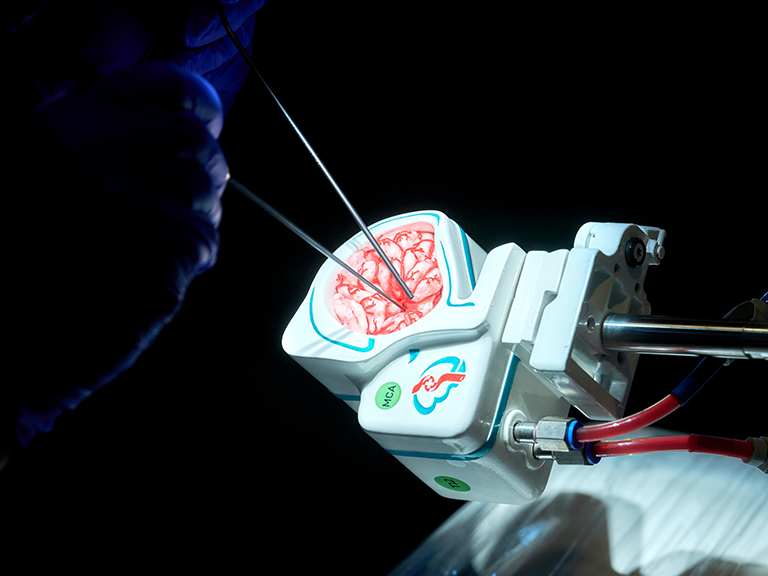
The 4D model, which realistically depicts not only the spatial dimensions but also the temporal dimension of the aneurysm in the skull because of the pulsation, stems from Raabe's idea – and Bervini's collaboration with Fredrick Johnson Joseph, who developed the hardware and software of the simulation robot for his doctoral thesis at the ARTORG Center for Biomedical Engineering at the University of Bern.
Almost two years ago, Joseph, who in the meantime has become a postdoctoral researcher, also founded a start-up company with Bervini called "SurgeonsLab", which he now also heads as CEO. "I am someone who works day and night," says Joseph. With their company, Joseph and Bervini want to distribute the new sophisticated training technology internationally.
Preparing upcoming operations
The company's 3D printers, which produce the 4D model of the aneurysm in the skull, are controlled by an algorithm in the cloud, Joseph explains. "This allows physicians from all over the world to upload the image data of an aneurysm," says Joseph. "Within a few days, we send them back a true-to-life image."
With this image, the specialists can then prepare for the upcoming operation – and, for example, tinker with the optimal placement of the clips. This preparatory work subsequently facilitated and accelerated the real operation. "The costs for the individual practice model should be more than offset by the savings resulting from the reduced operation time", says Joseph.

Joseph and Bervini have already won numerous prizes for the 4D simulator, such as the Ypsomed Innovation Prize worth 50 000 Swiss francs and the Venture Kick Award worth 150 000 Swiss francs. Diamantoula Pagkou and the other participants in the simulation workshop are also very taken with the simulation. "It works better than I expected," says Pagkou after the first two-hour hands-on block.
Enhanced patient safety
While Joseph is already thinking about other possible fields of application for the simulation robot (such as practising the surgical removal of tumours), Raabe is focusing on another aspect. "Neurosurgical training is currently very heterogeneous. We want to establish a high, worldwide standard," says Raabe. He expects that with improved planning and practice of the interventions, the risk of bleeding and other complications can be reduced. And in return, patient safety will increase during the delicate aneurysm operations.
The online magazine of the University of Bern

Subscribe to the uniAKTUELL newsletter
The University of Bern conducts cutting-edge research on topics that concern us as a society and shape our future. In uniAKTUELL we show selected examples and introduce you to the people behind them – gripping, multimedia and free of charge.