"We should not underestimate how important travel can be"
Emma Hodcroft of the Institute of Social and Preventive Medicine, using the Nextstrain sequencing platform she co-developed, has identified a new coronavirus variant (EU1) that spread rapidly in Europe last summer. Travel during summertime played an important role for the rise of EU1. Summer vacations are coming soon: How can we travel without too much risk?

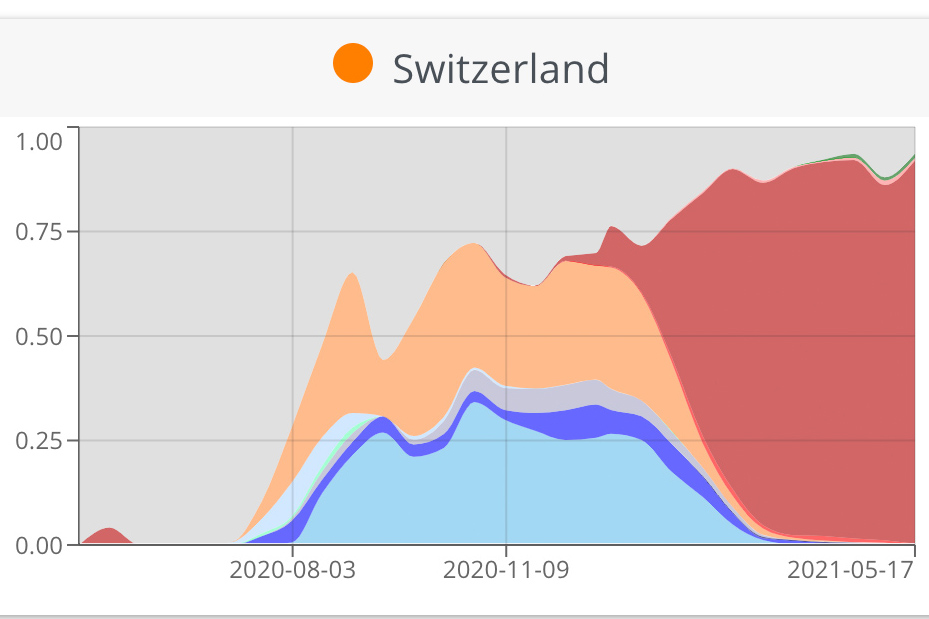
The really interesting thing about EU1 is that we first thought it might be more transmissible, because we could see how it was rising in frequency across Europe. But the more we started looking into it, we noticed that there was an association with travel. We believe that the real success of EU1 was the fact that it was able to take advantage of the many holidays and travel that happened last summer after lockdowns eased to spread across Europe unchecked for a few months at least. So EU1 showed that a variant can rise and become really prevalent without needing to be more transmissible. Even now that we do have variants that do seem to be more transmissible, it’s a reminder to not underestimate how influential travel can be, and that we have to keep that in mind when we see new variants.
In Switzerland, as we could show with Nextstrain, it peaked at about 30% of our sequences. We had a bit more of a mix of variants in Switzerland. We think that it was introduced multiple times from Spain in most countries in Europe, so probably many holiday makers came back from Spain carrying EU1. But then over time, EU1 became very common in other countries in Europe – so that meant that even when countries were saying: "Don’t travel to Spain anymore", unfortunately at that point, EU1 was not just in Spain. So it was travelling between other countries in Europe as well.
What works best when it comes to containment strategies regarding travelling?That’s really tough! But I think testing is really an easy way to help everyone to know if people are coming back with the virus. Most importantly, it informs people themselves. Because I think trust-based quarantine is hardest for people if they feel fine, and they think "I won’t have it, it’s OK if I go out". If people know that they have it, it’s much easier for them to realize: "I really have to stay home because I could infect someone".
It is tough for countries to decide: where do we want to have a quarantine and where not? How do we make sure the quarantine is really working the way we think it is, and is being effective? Making sure test-and-trace systems are watching out for travel cases is probably another one of the best ways. We’re never going to actually catch everyone who comes into the country, test every single person, or some of those tests may be false negatives. But if we have a good system in our country, to make sure that those infections don’t transmit, then they stop at that person. So that’s the next best thing: even when an infection arrives, we want to end it at one person.
We wanted something that is easy to say, easy to remember, something that people are already familiar with a little bit, but that it didn’t have a connotation with a country. That was one thing we tried to avoid, to reduce people saying the "Indian variant", "the South-African variant". I think Greek letters tick a lot of these boxes: they’re easy to say, used worldwide in math, physics and science, and they don’t make people think that the variant came from this one place, and that place is bad. We tried other options, like including just numbers: variant 1, variant 2,.. or to naming the variants like storms, after people’s names, or others, but there were downsides to each of these approaches, so we decided to use the Greek alphabet.
Do you think the Delta version could become also the dominant variant in Europe?I think it’s still a little bit too early to say. What’s happening with the Delta variant is a good reminder of what we’ve learned with EU1 – because at the moment we don’t see the Delta variant much in continental Europe, it seems to be mostly in the UK. One of the things that is really different there, is the number of strong connections to India, and many people arrived from India to the UK before the travel ban went in place. Just like with EU1, introductions make a difference. Now that doesn’t mean that the variant isn’t more transmissible, it could be more transmissible as well, but it makes it a little harder to predict whether this will be similar in Europe or maybe because we had fewer introductions, we manage to contain it more. I think at the moment we need more data before we can predict that.
We’re in a comfortable position here, but what happens when the Delta variant hits countries with no vaccines or poor infrastructure, like Nepal or countries in Africa?This is really where we should be trying to focus some more discussion and support. Especially in the west, in the US, in a lot of Europe, we’re reaching a point now where we’ve got a good vaccine roll out, and we’re expecting to have a large number of people vaccinated in the next month or two. That’s fantastic, but it’s so far from the case in so many countries around the world that are still at risk. And I would love to see and hear more governments starting to turn their attention to "OK, we’ve got things going pretty well in our country, how do we support other countries now? How can we extend the availability of vaccinations, how can we provide oxygen tanks in countries with outbreaks, or money for health care services?"
Because the thing is: this is a global pandemic, and we’ve seen what happens when variants arise in other countries - they can come to our country. Our restrictions are not perfect. And what we definitely don’t want to see is a variant arising that can make its way around vaccines. So the best strategy is to make it so that everyone can control their case numbers. Because we won’t really be safe from Sars-CoV-2 until everyone is able to keep those case numbers down.
I think that’s a great question, and it is a problem. One of the troubles with travel restrictions for example is that if we don’t have any sequences from a certain country, then of course it has no variants, so travel is unrestricted. Now I’m not saying we should restrict it entirely in these cases, but it’s just an illustration of the fact that no data necessarily doesn’t mean that there’s no problem. It just means that we don’t know.
Also, I think it would be really good to try and make a more coordinated global approach so that more countries have access to sequencing. Because if a new variant arises, we want to be able to start learning about this straight away, and not wait until it’s gone through three countries to the one that has a sequencer. That might be a point where it becomes really hard to contain, and where a lot of people might have been hospitalized or died. So the earlier we can learn about these things, the more countries have access to sequences, the much better informed we will be about what’s going on around the world when it comes to new variants and transmission.
What would you recommend if I wanted to travel to Spain or another country that is not at risk with my family in summer?I would definitely encourage people to get their vaccines, and if you can where you are, wait until two weeks after the second dose. That’s when you should have real effective immunity against Sars-CoV-2. Of course, that doesn’t mean that you should go around and kiss everyone you meet, but it really lowers your risk that you’ll be infected or bring something back.
Then just travel consciously: think about what are the things that you really want to do, and what things maybe can you live without doing this year? Maybe spend more time on the beach, and less time in a club. Maybe try and sit outside restaurants. And if you go somewhere, and it seems to be just too crowded – maybe in that country they let more people into a building than we do in Switzerland – you can always say: "This isn’t for me". It’s okay to change your mind and say "Let’s try and come tomorrow, we’ll come earlier, it will be less busy." So I think this summer really being flexible is something that we all can take advantage of. Thinking about how can we spend more time outside, and not doing something just because we said we’d do it, but because we feel it’s safe and we’re comfortable with it.
What about your summer plans: Will you visit your family in the UK or US?I’m not making any concrete plans at the moment, I’m hopeful especially because where my family is in the UK and the US, vaccination has been going really well, and cases in general have been contained. But I want to make sure that it’s safe and advisable before I get too excited. If it turns out that waiting is the best thing, I would rather do my part to keep things safe than to risk anybody. But I’ve got my fingers crossed!
About Emma Hodcroft
Since 2020, molecular epidemiologist Emma Hodcroft has been working as a postdoc at the Institute of Social and Preventive Medicine (ISPM) at the University of Bern. The 34-year-old studied biology at Texas Christian University, moved to the University of Edinburgh for her master's degree, and then completed a PhD and postdoc there on the genetic evolution of HIV. Hundreds of newspapers around the world covered her work on Nextstrain, an open-source platform that tracks the evolution of Sars-CoV-2 mutations. With more than 64,000 followers (as of early June), she is one of Switzerland's most followed researchers on Twitter.
About the author
Nathalie Matter is an editor at Media Relations and is responsible for health & medicine topics at the Communications & Marketing Department of the University Bern.